Treatment Overview
Fertility Preservation Counseling is a critical first step in helping cancer patients understand, plan, and protect their reproductive future before undergoing gonadotoxic treatments such as chemotherapy, radiation, or surgery. This counseling bridges oncology and reproductive medicine — offering individualized guidance on the safest, most effective fertility preservation options.
In Korea, fertility preservation counseling is highly developed, combining medical expertise, emotional support, and technological precision. Multidisciplinary teams, including oncologists, reproductive endocrinologists, fertility specialists, and psychological counselors, work together to provide clear information about available preservation strategies and the impact of cancer treatments on future fertility.
This approach empowers patients to make informed, time-sensitive decisions that align with both their medical and personal goals, ensuring that life-saving cancer therapy proceeds without sacrificing reproductive potential.
Purpose & Benefits
The purpose of fertility preservation counseling is to inform, support, and prepare patients for fertility protection prior to cancer treatment.
Key benefits include:
- Personalized fertility planning: Helps patients choose the most suitable preservation method based on age, cancer type, and treatment urgency.
- Education on fertility impact: Explains how chemotherapy and radiation affect ovarian reserve, hormone function, and reproductive health.
- Emotional reassurance: Provides psychological and emotional support during a stressful decision-making period.
- Informed decision-making: Ensures patients fully understand risks, benefits, timelines, and outcomes of available treatments.
- Oncology collaboration: Coordinates fertility interventions with cancer specialists to avoid delaying therapy.
- Long-term reproductive health management: Establishes a roadmap for fertility restoration after remission.
Korean fertility centers emphasize patient-centered care, focusing on both medical accuracy and emotional well-being throughout the process.
Ideal Candidates
Fertility preservation counseling is suitable for:
- Women and men diagnosed with cancer who are about to undergo chemotherapy, radiotherapy, or surgery that could impair fertility.
- Patients of reproductive age (teens to mid-40s) concerned about post-treatment fertility.
- Individuals with hormone-sensitive cancers, such as breast or ovarian cancer, needing specialized fertility planning.
- Prepubertal patients and their guardians, who require early guidance on available options like ovarian tissue preservation.
- Patients with recurrent or genetic cancer risk planning future family building.
- Couples seeking embryo cryopreservation before cancer therapy.
Fertility counseling is ideally conducted immediately after diagnosis, allowing time for informed fertility decisions before treatment begins.
Possible Risks & Challenges
While counseling itself is a safe and essential process, certain challenges can arise:
- Emotional overwhelm: Patients may feel anxious or conflicted about fertility decisions during cancer diagnosis.
- Time sensitivity: Limited time between diagnosis and treatment may restrict available preservation options.
- Financial constraints: Fertility preservation may not always be covered by insurance.
- Complex medical coordination: Requires seamless communication between fertility and oncology teams.
- Information overload: Patients may struggle to process complex medical data during stressful circumstances.
In Korea, counseling programs are structured to reduce these challenges through clear communication, psychological support, and rapid clinical coordination between departments.
Counseling Process & Clinical Approach
1. Initial Consultation and Medical Assessment
- Conducted immediately after cancer diagnosis or upon oncologist referral.
- Includes a review of cancer type, stage, treatment plan, and timeline.
- Fertility specialists evaluate ovarian reserve, hormonal profile, and reproductive health status.
2. Education on Fertility Risks
- Counselors explain how chemotherapy and radiation can damage reproductive organs and hormones.
- Information provided on expected outcomes for various treatment intensities.
- Discusses the difference between temporary and permanent infertility risks.
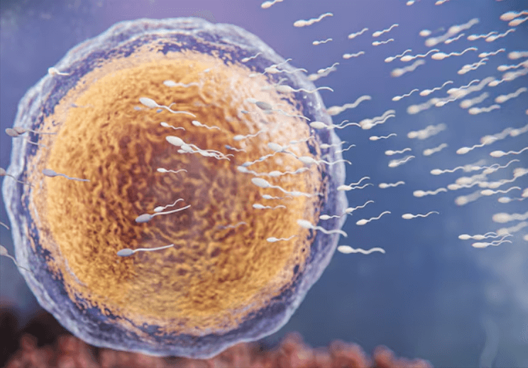
3. Fertility Preservation Options
- Detailed presentation of preservation methods such as:
- Oocyte cryopreservation (egg freezing)
- Embryo cryopreservation (with partner or donor sperm)
- Ovarian tissue cryopreservation (for urgent or prepubertal cases)
- Hormonal suppression therapy (GnRH agonists to protect ovarian function)
- Radiation shielding or ovarian transposition (for pelvic cancer cases)
- Discussion of expected success rates, timelines, and safety for each option.
4. Oncology Coordination
- Fertility and oncology teams collaborate to schedule preservation procedures without delaying cancer treatment.
- Modified stimulation protocols (such as random-start IVF) are planned if necessary.
5. Psychological & Emotional Support
- Trained counselors provide emotional support to help patients navigate fears and decisions.
- Patients receive mental health care to cope with the dual stress of cancer and fertility planning.
6. Financial Counseling
- Clear cost breakdown of procedures, storage fees, and follow-up care.
- Guidance on available government support or financial aid programs.
7. Documentation & Long-Term Planning
- Detailed medical documentation ensures long-term traceability of stored eggs, embryos, or tissue.
- Future fertility restoration strategies are outlined based on cancer prognosis and recovery trajectory.
Recovery & Aftercare
Following counseling and preservation procedures:
- Patients receive hormone monitoring and post-procedure follow-up to ensure recovery before cancer therapy begins.
- Oncologic follow-up ensures that fertility preservation does not interfere with cancer treatment.
- Psychological counseling continues throughout treatment and remission to address fertility concerns.
- After cancer recovery, fertility specialists provide delayed fertility restoration counseling to plan conception.
Korean fertility programs ensure that each patient’s journey is medically safe and emotionally supported from diagnosis through post-treatment fertility recovery.
Results & Effectiveness
Fertility preservation counseling in Korea leads to excellent patient understanding, satisfaction, and long-term fertility outcomes.
Observed benefits include:
- High patient participation rates: Most cancer patients offered counseling opt for preservation.
- Improved psychological readiness: Patients report reduced anxiety after clear fertility guidance.
- Optimal decision-making: Counseling ensures appropriate selection between oocyte, embryo, or tissue preservation.
- Seamless treatment coordination: Fertility interventions are completed within safe timeframes before therapy.
- Positive long-term outcomes: Many patients return post-recovery for fertility restoration and successful pregnancies.
- Enhanced quality of life: Patients feel empowered knowing their reproductive options are protected.
Korean counseling systems focus not only on fertility outcomes but also on the patient’s holistic well-being and future family planning goals.
Treatment Process in Korea
Step 1 – Oncology Referral & Rapid Scheduling
- Once a cancer diagnosis is made, the oncologist refers the patient to an oncofertility team for immediate counseling.
Step 2 – Multidisciplinary Evaluation
- Fertility, oncology, and endocrinology specialists assess reproductive risk and preservation options.
Step 3 – Counseling Session
- One-on-one counseling with fertility specialists, nurses, and psychologists.
- Education on procedures, timing, risks, and post-treatment fertility planning.
Step 4 – Decision & Procedure
- Based on medical urgency, patients undergo oocyte retrieval, tissue preservation, or hormonal protection before treatment.
Step 5 – Long-Term Follow-Up
- Continued counseling during and after cancer therapy.
- Fertility restoration planning once remission is confirmed.
Why Korea Excels in Fertility Preservation Counseling
- Integrated Oncofertility Networks: Collaboration between cancer hospitals and fertility centers for rapid coordination.
- Highly trained reproductive specialists: Experts in both fertility preservation and endocrine oncology.
- Personalized counseling programs: Tailored to patient age, diagnosis, and fertility goals.
- Advanced communication systems: Real-time scheduling to prevent delays in cancer care.
- Multilingual support for international patients: Comprehensive guidance in English, Chinese, and other languages.
- Psychological & emotional care integration: Ensures compassionate and holistic patient management.
This structured and empathetic model ensures patients receive accurate, timely, and empowering fertility guidance in even the most urgent circumstances.
Cost Range
The cost of fertility preservation counseling in Korea depends on the number of sessions, tests, and coordination services required. Approximate costs:
- Initial consultation & fertility assessment: USD 150 – 300
- Comprehensive oncofertility counseling package: USD 300 – 700
- Psychological counseling & support program: USD 100 – 200 per session
- Fertility preservation procedure coordination: Often included in the preservation package
Counseling fees are generally minimal compared to preservation procedures and are often incorporated into overall oncofertility programs in major Korean hospitals.
Popular Clinics in Korea
- CHA Fertility Center (Seoul, Bundang): Offers dedicated oncofertility counseling and personalized preservation plans.
- Maria Fertility Hospital: Provides multidisciplinary counseling and psychological support for cancer patients.
- MizMedi Women’s Hospital: Known for rapid counseling coordination and advanced preservation protocols.
- Hamchoon Women’s Clinic: Specializes in individualized fertility planning for oncology patients.
- Seoul Women’s Hospital: Provides international oncofertility counseling and comprehensive patient care.