If you’ve just received your male fertility test results, you might be wondering what the numbers mean—and more importantly, what to do next. Whether you underwent a semen analysis, hormone testing, or additional evaluations, understanding your results is the first step toward a successful fertility plan.
This guide breaks down how to interpret your male fertility test results and outlines clear next steps depending on your diagnosis.
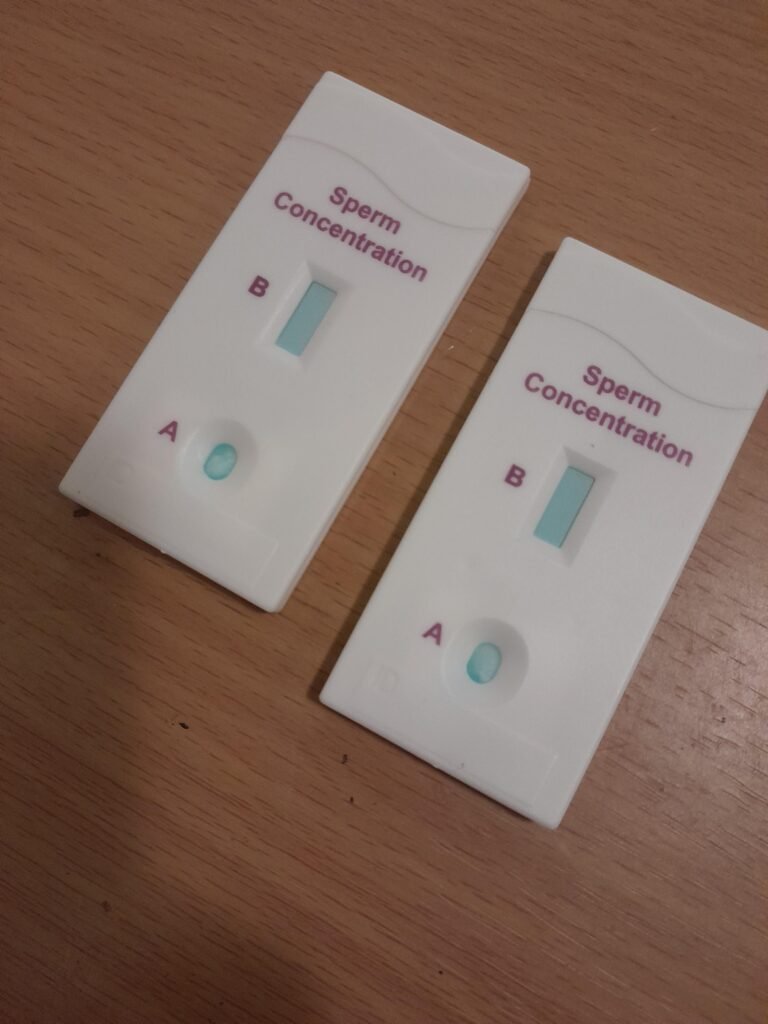
🧪 Common Male Fertility Tests and What They Evaluate
Before we dive into interpretation, here’s a quick overview of the most common tests used in male fertility evaluations:
| Test | What It Evaluates |
|---|---|
| Semen Analysis | Sperm count, motility, morphology, volume, and vitality |
| Hormone Testing | Levels of testosterone, FSH, LH, prolactin, TSH |
| Genetic Testing | Y-chromosome microdeletions, karyotype abnormalities |
| Ultrasound (Scrotal) | Structural issues (e.g., varicocele, obstruction) |
| DNA Fragmentation | Integrity of sperm DNA |
| Antisperm Antibody Test | Immune system reaction to sperm |
📊 Interpreting Your Semen Analysis Results
Semen analysis is the cornerstone of male fertility testing. Here’s how to interpret each parameter based on World Health Organization (WHO) standards:
| Parameter | Normal Range | What It Means |
|---|---|---|
| Sperm Count | ≥ 15 million/mL | Lower counts (oligospermia) may reduce fertility |
| Motility | ≥ 40% moving sperm | Poor motility (asthenozoospermia) affects sperm movement |
| Progressive Motility | ≥ 32% | Indicates ability of sperm to reach the egg |
| Morphology | ≥ 4% normal forms | Lower percentages (teratozoospermia) may impair fertilization |
| Volume | ≥ 1.5 mL | Low volume may suggest ejaculatory duct issues |
| Vitality | ≥ 58% live sperm | If low, suggests poor sperm survival |
| pH Level | 7.2–8.0 | Out-of-range pH may suggest infection or obstruction |
| White Blood Cells | < 1 million/mL | High count may indicate inflammation or infection |
If one or more values are outside the normal range, this doesn’t automatically mean you’re infertile—it just means further evaluation is necessary.
🧬 Interpreting Hormone Test Results
Your hormone levels reflect how well your brain and testes are communicating to produce sperm.
| Hormone | Normal Range (may vary slightly) | What It Suggests if Abnormal |
|---|---|---|
| FSH | 1.5–12.4 mIU/mL | High = poor sperm production; low = pituitary problem |
| LH | 1.7–8.6 mIU/mL | High = testicular failure; low = hormonal signaling issue |
| Testosterone | 300–1,000 ng/dL | Low = affects libido, sperm production |
| Prolactin | 2–18 ng/mL | High = may signal pituitary tumor or hormonal imbalance |
| TSH | 0.4–4.0 mIU/L | High/low = thyroid issues affecting fertility |
⚠️ What Abnormal Results Might Mean
| Finding | Possible Diagnosis | Next Step |
|---|---|---|
| Azoospermia (no sperm) | Blockage, genetic issue, testicular failure | Ultrasound, hormone tests, genetic testing |
| Oligospermia | Low sperm count | Lifestyle changes, repeat testing, hormone panel |
| Asthenozoospermia | Poor motility | Antioxidant therapy, varicocele evaluation |
| Teratozoospermia | Poor morphology | DNA fragmentation, ART considerations |
| High FSH, low testosterone | Testicular failure | Consider sperm retrieval and ICSI |
| Normal semen but infertility | May suggest female factor or sperm DNA damage | Partner testing, DNA fragmentation |
🔄 What to Do After Abnormal Results
1. Repeat the Test
- Many semen abnormalities are temporary due to illness, stress, or lifestyle.
- Wait 2–3 weeks and repeat to confirm.
2. Lifestyle Modifications
If you smoke, drink heavily, use drugs, or are exposed to heat/toxins, these can all lower fertility. Key changes:
- Avoid hot tubs, saunas, and laptops on your lap
- Maintain a healthy weight
- Eat a nutrient-rich, antioxidant-heavy diet
- Take supplements (zinc, CoQ10, vitamin C, folate—ask your doctor)
3. Further Testing
Depending on your initial results, your doctor may order:
- Scrotal ultrasound to check for varicocele or obstruction
- Hormone or genetic testing
- Sperm DNA fragmentation analysis
- Antisperm antibody test
4. Consult a Specialist
A reproductive urologist can help diagnose and treat the cause of male infertility. They may recommend:
- Surgical correction (e.g., varicocele repair)
- Hormonal therapy (e.g., Clomid, hCG)
- Sperm retrieval techniques (e.g., TESE, PESA)
- ART (assisted reproductive technologies)
🧬 Assisted Reproductive Options
Even if your results are significantly abnormal, you may still be able to have biological children through ART:
| Option | When It’s Used |
|---|---|
| IUI (Intrauterine Insemination) | Mild sperm abnormalities; moderate motility or count |
| IVF (In Vitro Fertilization) | Moderate to severe sperm issues |
| ICSI (Intracytoplasmic Sperm Injection) | Severe sperm defects, azoospermia (with retrieval) |
| Sperm retrieval | No sperm in ejaculate, but production confirmed |